by Jocelyn Pederson
“A rose by any other name would smell as sweet,” Juliet proclaims. However, if Juliet had been born today she might have said: “Xanax by any other name is still Xanax”. This concept, unfortunately, seems to elude legislators, the media and medical professionals alike. All the buzz these days seems to be about Xanax (Alprazolam). Haven’t you heard about all the college students abusing Xanax? Isn’t it terrible how often Xanax is involved in all those overdose deaths? Some places are even taking legislative action against Xanax. In Alabama, for instance, the Board of Medical Examiners has requested to have Xanax changed from a Schedule IV controlled substance to a Schedule II, alongside such substances as Morphine, Fentanyl, and Adderall.
Why does Xanax get all the glory? Is it because Xanax is more dangerous and addictive than its fellow benzodiazepines Ativan (Lorazepam), Klonopin (Clonazepam), Valium, etc.? There doesn’t seem to be any scientific evidence to support the idea. Perhaps it’s simply because Xanax is prescribed more frequently than its lesser known counterparts. This may be due in part to doctor preference or due to the half-life of Xanax which requires more frequent dosing. It could also be due to the celebrity of the drug itself. I challenge you to watch the latest blockbuster film or reality TV show without hearing some reference to Xanax or “Xannies”. Even daytime TV darling Kelly Ripa glibly announced that she took “half a Xanax” to help her deliver her acceptance speech at the GLAAD Awards, a statement which was met with raucous applause by the audience.
While any effort to generate awareness and potentially curb the benzodiazepine epidemic is commendable, we have to ask ourselves, is Xanax just the scapegoat in this situation? Will legislative action and media attention for only one benzodiazepine out of so many make any difference? If we look at the history of this problem we see the answer to that question is a resounding “NO”. Remember Valium? “Mother’s little helper,” as it was endearingly termed by the Rolling Stones, was once the most prescribed drug in the US with more than 2.3 billion pills sold per year at its zenith. All of a sudden there was a Valium epidemic and the public was both frightened and angry. In comes Pfizer to save the day (along with other manufacturers) to provide us with “safer”, shorter-acting benzodiazepines that were less addicting, like Xanax! Today we are shocked to discover that Xanax is every bit as bad as the disgraced Valium. Not to worry, Klonopin, Ativan and the others will still be there to pick up the slack…and so the merry goes round and round.
Klonopin and Ativan do not have the same reputation as Xanax and Valium, but they are no less destructive. Tens of thousands of people in the US seek treatment for tranquilizer withdrawal every year. However, only about half of them are there because of Xanax.
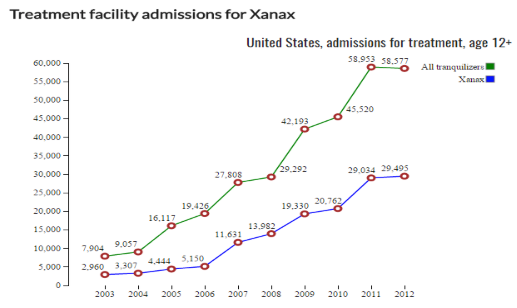
Image from drugabuse.com
Most people have heard of Xanax but have no idea what a benzodiazepine is, or that they might be currently taking one. This lack of awareness means that patients who are prescribed Restoril (Temazepam) for insomnia, Klonipin for anxiety or Ativan for restless leg syndrome are often unaware that they are taking a potentially dangerous and addictive substance that is only meant for short term use, approximately 2-4 weeks. It’s easy to see how this can turn many people into accidental addicts.
It’s not just about addiction though. People can die if they suddenly stop taking benzodiazepines, even when they are taken as prescribed by a doctor. Let’s get something straight once and for all, while you can die from overdosing on opiates, death is not a side effect of opiate withdrawal. Benzodiazepines, on the other hand, have that listed right there on the package insert. Benzodiazepines are unlikely to kill you if you take too many. However, if you suddenly stop taking one or let your prescription run out before you can get a refill, your life could be in danger. Jesse Jacobs, Marshal Carman, John Patrick Walter, Gregory Lee Hill, Tyler Tabor, Sean Levert all died in jail after being denied their prescriptions for Klonopin and Xanax. Some of these men were booked for things like unpaid parking tickets or were only serving a sentence of a few weeks. Where is the media outcry? The Twitter storms? Are doctors warning patients that their anti-anxiety/anti-depressant medication could potentially be a life sentence?
Then there are the other potential life threatening and life altering problems related to benzodiazepine use. How many women are aware that their Ativan is teratogenic and can cause miscarriage and birth defects in the first 8 weeks before they even realize they are pregnant and can get safely off? Studies have shown that long-term benzodiazepine use can also lead to increased infections, car accidents, Alzheimer’s, diabetes, cancer, suicide, and the list goes on and on. This is a problem that goes well beyond addiction and it’s not exclusive to Xanax.
If there is going to be any hope of reducing the potentially hundreds of thousands of benzodiazepine-related deaths every year then we have to look at the entire class of benzodiazepine drugs just as we do opiates. It would almost seem ridiculous for legislators to put forward a bill to address the “Codeine epidemic”. It’s every bit as silly to focus all our attention only on Xanax.
When actor Heath Ledger died 2 opiates and 3 benzodiazepines were found in his in his system including Valium (diazepam), Restoril (temazepam) and Xanax (alprazolam). While this may seem excessive, it is not uncommon for people (including many celebrities who have died) to be prescribed multiple different benzodiazepines along with opiates for different problems such as insomnia, pain, and anxiety. Deaths like this are why the FDA recently issued a black box warning against combining opiates and benzodiazepines. But what is being done about the irresponsible and off-label prescribing that continues to flood benzodiazepines into our homes and onto the streets?
Even with increased warnings, benzodiazepine prescriptions continue to steadily increase year after year. The current focus by the medical community, media, and legislators on Xanax will not create the kind of change that is needed to change the course of the benzodiazepine epidemic. If social media is an indication of anything, it’s that Xanax can more than easily be replaced by:
Ativan:
Klonopin:

Or even the Z-drug Ambien (similar to benzodiazepines):
We need to stop pretending that what we have is a Xanax problem. I get it, it’s convenient to have a scapegoat. It means we can shift the blame from ourselves onto something else. Nobody wants to consider that the most popular and profitable drugs on the market today are part of a silent epidemic that affects anywhere between 3 and 16 million Americans every year. Maybe we’re afraid to shine a light on the benzo problem until the next class of wonder drugs has come out to take their place. After all, benzodiazepines are considered to be more dangerous and difficult to withdraw from than heroin. Who has time for that? Perhaps doctors are reticent to admit that 40-90% of the time benzodiazepine prescriptions are written, there is no clear medical reason for doing so. Whatever the reason, if the Valium epidemic taught us anything, it’s that Xanax is not the answer to our problem.

This entry was submitted by guest blogger Jocelyn Pederson. She has a benzodiazepine help channel on YouTube called Benzo Brains and currently runs the Facebook group Keto 4 Benzo Recovery. Jocelyn lives in Utah with her husband and two children.
Blog posts are essays submitted by a diverse group of writers engaged in benzodiazepine activism and awareness. Posts may consist of opinion pieces, creative writing, personal stories and/or more scientific research-based writings, etc. W-BAD encourages all bloggers to cite sources within their writing where possible and also encourages public discussion and respectful debate on topics. Please always do your own research and read W-BAD’s Disclaimer, as blog post content should never be a substitute for medical oversight. If you are interested in submitting a blog post to W-BAD, please Contact Us.

Excellent article Jocelyn! Indeed looks like Xanax is the new Valium. A “scapegoat” for sure. My friend’s doctor suddenly wants to take him off his Xanax of 12 years (while disregarding his plea to stay on). He’s 82 and scared he might not survive withdrawal. We asked: “Why Xanax? Is he the only patient your’e taking off Xanax?” Her responses were, “There’s new regulations, Xanax has bad side effects, I want to keep my licence, I’m taking all my patients off Xanax.” She wants him off Xanax soon and then onto Klonopin to taper off that. Keep in mind, he was never warned from the start, when first prescribed about the inevitable dependency to come, nor of the life threatening withdrawals should he attempt to come off, and now it’s about her licence. She’s not interested in liquid titrating him off in a more humane way. And staying on is not an option. She simply wants him off. It’s about the Xanax.
All benzodiazepines can cause dependency, adverse effects and a withdrawal syndrome, but they’re not all the same. If they were, we wouldn’t need Ashton’s diazepam substitution tapering protocol.
The reasons why Xanax gets such a bad rap are possibly similar to the reasons why Halcion (triazolam) was banned in Britain years ago. They’re both triazolobenzodiazepines, which are arguably more dangerous than classic BZDs.
See this post for the science behind this: http://worldbenzoday.org/xanax-klonopin-nickname-origins/