
Socioeconomic costs of long-term as-prescribed benzodiazepine use
Socioeconomic costs incurred due to the prevalent outright ignoring of manufacturer guidelines and haphazard, irresponsible prescription of benzodiazepines (BZs) long-term is immense, albeit difficult to truly quantify. Some socioeconomic costs of long-term, as-prescribed benzodiazepine (and Z-drug) use is as follows:
Increased risk of accidents – traffic, home, work.
Traffic: In Ireland, the gardai (law enforcement) have implemented new machines which will test motorists for benzodiazepines and sleeping pills (among other drugs). This will not, however, affect people taking BZs as-prescribed who are driving, in spite of people using them as directed still being at increased risk for motor vehicle accidents due to the BZ’s adverse effect profile (detailed below).
Falls and accidents in the elderly: Older people are more sensitive than younger people to the central nervous system depressant effects of benzodiazepines. Benzodiazepines can cause confusion, night wandering, ataxia (loss of balance), in the elderly and should be avoided wherever possible, as these symptoms can lead to an increased risk of falls and accidents in the elderly.
In general, even in non-elderly individuals, benzodiazepines and Z-drugs (sleeping pills) can cause sedation, confusion, memory loss, drowsiness, poor concentration, incoordination, muscle weakness, dizziness, and mental confusion which can all contribute to an increased risk for accidents.
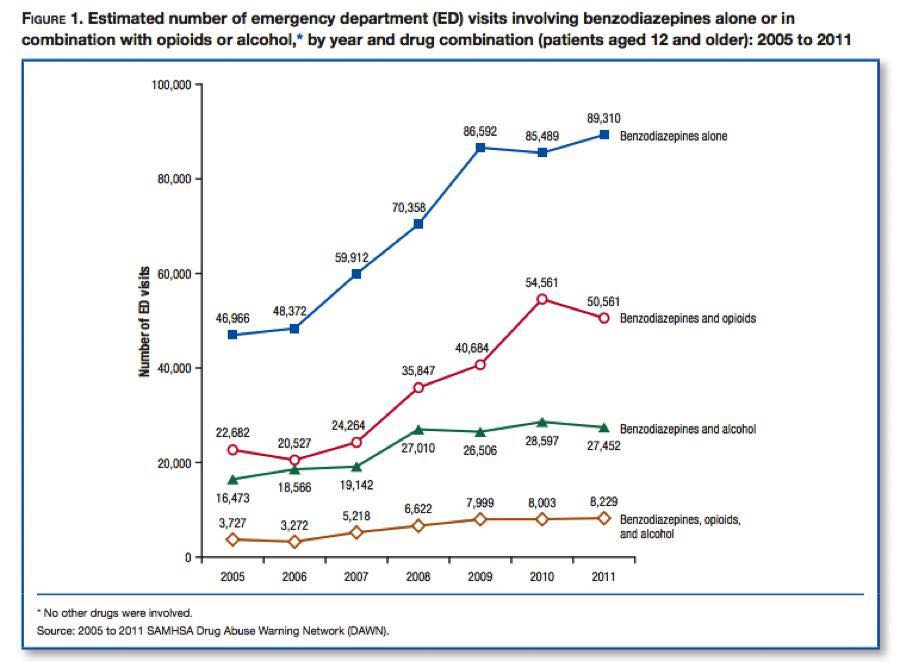
Increased risk of fatality from overdose if combined with other drugs.
From The Ashton Manual: “Benzodiazepines have additive effects with other drugs with sedative actions including other hypnotics, some antidepressants (e.g. amitriptyline [Elavil], doxepin [Adapin, Sinequan]), major tranquilizers or neuroleptics (e.g. prochlorperazine [Compazine], trifluoperazine [Stelazine], chlorpromazine [Thorazine], haloperidol (Haldol), pimozide [Orap]), anticonvulsants (e.g. phenobarbital, phenytoin [Dilantin], carbamazepine [Atretol, Tegretol], valproic acid [Depakote], Lamotrigine [Lamictal]), sedative antihistamines (e.g. diphenhydramine [Benadryl], promethazine [Phenergan]), opiates (heroin, morphine, meperidine), and, importantly, alcohol. Patients taking benzodiazepines should be warned of these interactions. If sedative drugs are taken in overdose, benzodiazepines may add to the risk of fatality.”
In 2016, in the US, the FDA issued a release requiring strong warnings for opioid analgesics, prescription opioid cough products, and benzodiazepine labeling related to serious risks and death from combined use.
Relevant News Articles from Around the Globe on this Topic:
The Washington Post: Overdoses on anti-anxiety meds such Valium and Xanax are on the rise
Reuters: Benzodiazepine prescriptions, overdose deaths on the rise in U.S.
CNN: Benzodiazepine overdose deaths soared in recent years, study finds
Traci Green and Josiah Rich: Rhode Island is poised to stop epidemic
The Age: Prescription drug deaths in Victoria eclipse road fatalities
Irish Examiner: Legal drugs cause 75% of poisoning deaths
Increased risk of attempted suicide, especially in depression.
In 1988 the Committee on Safety of Medicines in the UK recommended that “benzodiazepines should not be used alone to treat depression or anxiety associated with depression. Suicide may be precipitated in such patients”.
From The Ashton Manual: “Long-term benzodiazepine users, like alcoholics and barbiturate-dependent patients, are often depressed, and the depression may first appear during prolonged benzodiazepine use. Benzodiazepines may both cause and aggravate depression, possibly by reducing the brain’s output of neurotransmitters such as serotonin and norepinephrine (noradrenaline). However, anxiety and depression often co-exist and benzodiazepines are frequently prescribed for mixed anxiety and depression. Sometimes the drugs seem to precipitate suicidal tendencies in such patients.”
Increased risk of aggressive behavior and assault.
From The Ashton Manual: “Benzodiazepines occasionally cause paradoxical excitement with increased anxiety, insomnia, nightmares, hallucinations at the onset of sleep, irritability, hyperactive or aggressive behaviour, and exacerbation of seizures in epileptics. Attacks of rage and violent behaviour, including assault (and even homicide), have been reported, particularly after intravenous administration but also after oral administration. Less dramatic increases in irritability and argumentativeness are much more common and are frequently remarked upon by patients or by their families. Such reactions are similar to those sometimes provoked by alcohol. They are most frequent in anxious and aggressive individuals, children, and the elderly. They may be due to release or inhibition of behavioural tendencies normally suppressed by social restraints. Cases of “baby-battering”, wife-beating and “grandma-bashing” have been attributed to benzodiazepines.”
Increased risk of shoplifting and antisocial behaviors
This may be due to a phenomenon called ‘Intoxication anosognosia’ (or ‘medication spellbinding’): “Intoxication anosognosia (medication spellbinding) is an expression of this drug-induced mental disability. Intoxication anosognosia causes the victim to underestimate the degree of drug-induced mental impairment, to deny the harmful role that the drug plays in the person’s altered state, and in many cases compel the individual to mistakenly believe that he or she is functioning better. In the extreme, the individual displays out-of-character compulsively destructive behaviors, including violence toward self and others.”
Contributions to marital/domestic disharmony and breakdown due to emotional and cognitive impairment.
From The Ashton Manual: “‘Emotional anaesthesia’, the inability to feel pleasure or pain, is a common complaint of long-term benzodiazepine users. Such emotional blunting is probably related to the inhibitory effect of benzodiazepines on activity in emotional centres in the brain. Former long-term benzodiazepine users often bitterly regret their lack of emotional responses to family members – children and spouses or partners – during the period when they were taking the drugs. Chronic benzodiazepine use can be a cause of domestic disharmony and even marriage break-up.”
Contributions to job loss, unemployment, loss of work through illness.
When in tolerance withdrawal or while tapering and in post-acute withdrawal, many patients who use(d) BZs as prescribed and long-term become disabled and unable to continue working. Where these individuals were former taxing-paying, contributing members to society, they are, instead, often left collecting benefits (such as Social Security Disability in the US) due to the severity of their condition leaving them unable to garner income as a result of the iatrogenic BZ damage incurred.
Many BZ-injured patients, due to disability leading to job loss, wind up collecting government benefits (like Social Security Disability, food stamps, housing assistance, Medicare, and Medicaid, for example, in the United States and similar programs in other countries). What would be productive, functional, tax-paying members of society are now costing tax-payer dollars due to this medical scandal. The financial impact is wide-reaching.
Cost of hospital investigations/consultations/admissions.
In addition to the cost of office visits (to the patient, taxpayer and/or insurance companies) for refills and monitoring of long-term prescription of BZs, additional costs are incurred due to doctor and hospital visits for tolerance withdrawal from, adverse effects of, and/or withdrawal syndromes from BZs. Often times, tolerance withdrawal symptoms, adverse effects and/or withdrawal syndromes are misdiagnosed as other illnesses and/or psychiatric conditions which lead to even more costly investigations, unnecessary medications, and/or treatments.
Insurance companies (or services like the NHS in the UK where there is universal healthcare) are, no doubt, paying and wasting countless millions of dollars senselessly due to benzodiazepine prescription. They not only pay for the initial repeat prescriptions and doctor visits which cause the iatrogenic dependency but then are stuck footing the bill for the increased use of services and drain on the medical system during the time of benzodiazepine tolerance and withdrawal. Any insurance company (or medical service, like the NHS) would be foolish, from a cost-benefit standpoint, not to examine this problem and then enforce a restriction on the duration for which they will pay for benzodiazepine prescriptions (e.g., less than 2 weeks).
Adverse effects in pregnancy and in the newly born.
From The Ashton Manual: “Benzodiazepines actively cross the placenta and, when taken regularly during pregnancy (even in therapeutic, prescribed doses) can cause neonatal complications. The foetus and neonate metabolise benzodiazepines very slowly, and appreciable concentrations may persist in the infant up to two weeks after birth, resulting in the “floppy infant syndrome” of lax muscles, oversedation, and failure to suckle. Withdrawal symptoms may develop after about two weeks with hyperexcitability, high-pitched crying and feeding difficulties. Benzodiazepines in therapeutic doses appear to carry little risk of causing major congenital malformations. However, chronic maternal use may impair foetal intrauterine growth and retard brain development. There is increasing concern that such children in later life may be prone to attention deficit disorder, hyperactivity, learning difficulties, and a spectrum of autistic disorders.”
Dependence potential (therapeutic).
Psychological and physical dependence can develop within a few weeks or months of regular or repeated use. There are several overlapping types of benzodiazepine dependence.
Note: Benzodiazepines are potentially addictive drugs as well and some individuals do abuse them. This also adds to socioeconomic costs, but will not be discussed in further detail as W-BAD’s mission is to solely focus on injuries and illness resulting from the as-directed use (with no history of abuse).
The cost of prescriptions.
The costs of the prescriptions are incurred by the patient (in areas like the US, where individuals sometimes incur some out-of-pocket costs for medications), insurance companies, and/or the taxpayers (in areas where there is universal healthcare). In 2013, in the US, Medicare paid for nearly 40 million tranquilizer prescriptions.
The cost of litigation.
Benzodiazepine Litigation ended owing to the withdrawal of Legal Aid Board funding. Over £50 million pounds was spent on legal aid and by the drug companies.
Litigation costs could also include costs incurred where patients sue their prescribers for malpractice, costs incurred where litigation occurs due to criminal behavior on the part of individual’s adversely influenced by BZs to commit crimes, etc.
These social and economic costs could be easily curbed if global governing bodies would pass some very simple legislation that would require adherence on the part of medical providers, similarly to what is currently being proposed in Massachusetts with Bill H.3594. More simply, the problem could be curbed in two ways: 1. By not creating more newly iatrogenically dependent patients by ceasing the long-term prescription of benzodiazepines near-altogether 2. By working with and creating services for already dependent patients in order to assist them in tapering off slowly and properly to allow them to discontinue use permanently. Tragically, without change, the current state of affairs, where medical prescribers go on prescribing long-term (often times without informed consent given to the patient of the risks and dangers of doing so) and where already-dependent patients have little or no access to withdrawal advice or support services, will persist.
In this short video (5:23), a W-BAD grassroots campaigner discusses some of the socioeconomic costs of BZs, as noted in The Ashton Manual:
Click on CC for captions in English. To contribute translations of this video in another language, click here.
Source: The Ashton Manual
Additional Reading:
Mad in America: Sweeping Benzos Under the Carpet
BBC News: Sleeping pills ‘linked to increased death risk’
